Value-based care is a healthcare model that prioritizes patient outcomes and quality of care over the volume of services provided. By exploring the history of value-based care, we can see how healthcare has evolved to improve patient well-being and efficiency. This article will cover the key milestones and reforms that have shaped value-based care.
Key Takeaways
Value-based care emphasizes improving health outcomes and sustainability, moving away from traditional fee-for-service models.
Legislation such as the Affordable Care Act has significantly advanced value-based care by promoting initiatives like Accountable Care Organizations and alternative payment models.
Technological advancements, including data analytics and personalized medicine, play a crucial role in enhancing the efficacy of value-based care by facilitating better patient management and treatment outcomes.
Early Beginnings of Value-Based Care
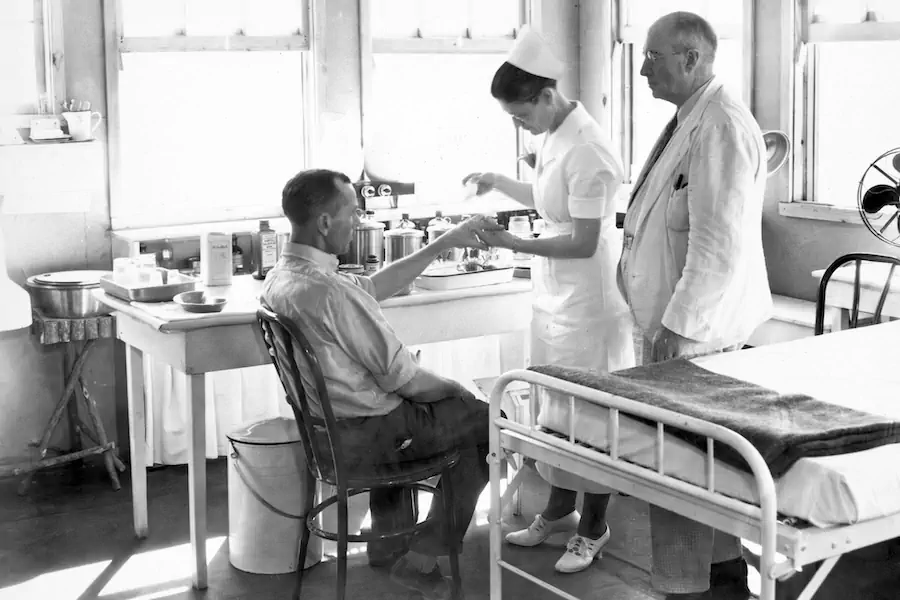
The concept of value-based care finds its roots in the early 20th century, drawing on ideas that aimed to improve health outcomes and ensure sustainability in healthcare. The limitations of the fee-for-service model, which often led to unsustainable costs and disparities in care quality, became increasingly evident. In response, value-based care introduced a focus on health outcomes per dollar spent, aiming to enhance patient well-being and the overall sustainability of the healthcare system.
One of the early advocates for outcomes measurement and accountability was Dr. Ernest Codman. His pioneering work laid the foundation for the principles of value-based care we see today. Codman’s emphasis on tracking patient outcomes and holding providers accountable for the quality of care delivered was a significant step towards the development of value-based care programs.
Value-based care has continually evolved, influenced by various models and reforms that sought to address the shortcomings of traditional healthcare delivery. Understanding the early influences that set the stage for value-based care is crucial when exploring its brief history.
The Influence of Managed Care
Managed care emerged in the mid-20th century as a response to rising healthcare costs, laying the groundwork for future healthcare reforms. The establishment of Health Maintenance Organizations (HMOs) aimed to enhance preventive care and control costs through a fixed annual payment model. This approach incentivized healthcare providers to focus on cost efficiency and preventive measures, setting the stage for value-based care models in healthcare.
Emphasizing cost control and preventive care, managed care models paved the way for alternative payment models and accountable care organizations. These early efforts to improve the healthcare system’s efficiency and effectiveness were crucial in shaping the future of value-based care.
The Role of Medicare and Medicaid Services
The establishment of Medicare and Medicaid in the 1960s marked a significant milestone in the history of value-based care. These programs were designed to provide healthcare access to the elderly and low-income populations, forming a vital part of the social safety net. Medicare’s primary goal was to ensure healthcare for older adults, while Medicaid aimed to assist those with limited financial resources.
Early on, Medicare and Medicaid began linking healthcare payments to service quality, moving beyond the purely fee-for-service model. This transformation set the stage for a broader adoption of value-based care, emphasizing the importance of outcomes over the volume of services delivered.
This shift promoted the principles of value-based care, encouraging providers to deliver high-quality care.
Evolution Through Policy and Reform
The evolution of value-based care has been significantly influenced by policy and reform. The introduction of Health Maintenance Organizations in the 1970s marked the beginning of a shift from volume to value in healthcare. This shift aimed to enhance the alignment of healthcare delivery with patient experiences, focusing on improving health outcomes. Value-based care emphasizes aligning healthcare provider incentives with patient health outcomes, promoting better care and cost efficiency.
Healthcare providers have faced significant challenges in implementing value-based care due to the complexity and potential financial risks associated with new payment models. However, the continuous adaptation of innovative payment models has allowed value-based care to evolve and better meet the needs of patients and providers.
Value-based care is adapting to new payment models that incentivize preventive care and chronic disease management. Key policies and reforms have played a crucial role in this evolution, driving the transformation of healthcare delivery through value based care (VBC).
The Affordable Care Act (ACA)
The Affordable Care Act (ACA) has been a pivotal policy in the development of value-based care. The ACA established the Center for Medicare and Medicaid Innovation to develop new payment models. This initiative was crucial in promoting value-based care and encouraging healthcare providers to focus on improving patient outcomes and controlling costs.
One significant healthcare model initiated by the ACA was the Accountable Care Organizations (ACOs). Introduced by President Obama in 2011, ACOs were designed to coordinate care for their members and focus on delivering high-quality health services while controlling costs. The ACA’s support for ACOs and other value-based care initiatives has been instrumental in advancing the principles of value-based care.
The CHIP Reauthorization Act
The CHIP Reauthorization Act has played a critical role in promoting value-based care initiatives for children’s health. Providing funding for children’s health services and promoting access to necessary healthcare, the CHIP Reauthorization Act has expanded value-based care and emphasized quality improvement initiatives for children.
The act has also facilitated initiatives targeting chronic disease prevention and improving birth outcomes for children, further supporting the principles of value-based care.
Introduction of Alternative Payment Models
The Medicare Access and CHIP Reauthorization Act (MACRA) established new payment systems that emphasize quality over quantity in healthcare delivery. These alternative payment models (APMs) incentivize providers to prioritize quality and cost-effectiveness, moving away from traditional fee-for-service models.
MACRA’s framework for alternative payment models has been crucial in advancing value-based care and promoting better patient outcomes.
Significant Programs and Initiatives
Several significant programs and initiatives have shaped the concept of value-based care, including Medicare, the Affordable Care Act, and technological advancements. These initiatives have decreased hospital readmissions, signaling better management of patient health and chronic conditions. Patients under value-based care programs often experience fewer hospital admissions compared to traditional care models, highlighting the effectiveness of these programs.
Value-based care has improved the management of chronic conditions, leading to better patient outcomes and fewer hospitalizations. The continuous development of innovative models in value-based care aims to enhance patient outcomes and further reduce unnecessary healthcare expenditures.
Accountable Care Organizations (ACOs)
Accountable Care Organizations (ACOs) are designed to coordinate care for their members and focus on delivering high-quality health services while controlling costs. The primary goals of accountable care organizations include improving patient outcomes through coordinated care, reducing unnecessary healthcare expenditures, and enhancing the overall quality of care delivered. One particular model that underpins the structure of ACOs is the ACO REACH Model, which emphasizes partnerships and integrated care strategies.
Bundled Payments for Care Improvement (BPCI)
The Bundled Payments for Care Improvement (BPCI) initiative emphasizes a single payment for all services delivered during an episode of care. This approach encourages hospitals and providers to deliver efficient care by offering a single payment for a group of related services, promoting cost efficiency and high-quality care.
The BPCI initiative includes four models that link payments for services during a patient’s care episode, further incentivizing healthcare providers to focus on coordinated and efficient care delivery. Taking on financial responsibility for the entire episode of care, organizations within the BPCI program are encouraged to collaborate and deliver better patient outcomes.
Medicare Advantage Plans
Medicare Advantage was developed in 1982, allowing beneficiaries to access HMOs with capitated payments, leading to improved patient outcomes. These plans often include value-based care models that incentivize healthcare providers to focus on quality over the quantity of services rendered.
Medicare Advantage plans typically combine coverage for hospital and outpatient services, supporting value-based care principles and enhancing care coordination. These plans may also offer additional services and benefits not typically covered by traditional Medicare, aligning with the principles of value-based care and improving patient satisfaction and health outcomes.
Impact on Healthcare Providers and Patients
The shift from volume-based to value-based care has been driven by various legislative actions aimed at improving patient outcomes and reducing costs. Value-based care programs focus on enhancing patient satisfaction and promoting better health outcomes, often linked to improved patient satisfaction and better health outcomes.
Technological innovations such as mobile health, telemedicine, and AI are pivotal in enhancing the efficiency of value-based care. Data analytics enable healthcare providers to track patient outcomes and improve care coordination through informed decision-making.
Technological tools like electronic health records (EHRs) facilitate better data management and communication in value-based care.
Financial Incentives for Providers
In value-based models, providers can potentially earn higher reimbursements by demonstrating improvements in patient outcomes.
Providers participating in value-based care models can receive bonuses based on the quality of care delivered, which encourages better patient management.
These financial rewards for delivering high-quality care align provider incentives with patient health outcomes.
Meeting quality benchmarks, providers in value-based care models can receive financial rewards, further motivating them to focus on improving patient outcomes and delivering high-quality care through quality measures.
Improvements in Patient Outcomes
Alternative payment models are increasingly linked to higher quality care and improved patient outcomes. Value-based care models focus on improving patient outcomes and reducing unnecessary costs in the healthcare system. Emphasizing preventive care and better management of chronic conditions, these models improve overall health outcomes and patient satisfaction.
The focus on reducing unnecessary healthcare costs and enhancing patient care coordination leads to significant improvements in patient outcomes, demonstrating the effectiveness of value-based care programs.
Challenges and Opportunities
Healthcare providers face various challenges in the transition to value-based care, including navigating new payment models and aligning incentives. The complexity of value-based care programs and the potential financial risks associated with new payment models can be daunting for providers. However, addressing these challenges is crucial for leveraging the full potential of value-based care opportunities.
Innovation and collaboration among healthcare providers, payers, and technology developers can create new solutions and improve care delivery. Working together, stakeholders can overcome challenges and enhance the effectiveness of value-based care programs, leading to better patient outcomes and cost savings.
The Role of Technology in Advancing Value-Based Care
Technology plays a crucial role in supporting the implementation and success of value-based care. Key technological advancements, such as artificial intelligence, predictive analytics, and personalized medicine, are expected to facilitate better health outcomes and cost efficiencies. These innovations enable healthcare providers to deliver more precise and effective treatments, ultimately enhancing patient outcomes.
One of the significant challenges in value-based care is the need for better data sharing among healthcare providers to support value-based initiatives. Leveraging technology and healthcare systems can improve data management and communication, leading to more coordinated and efficient care delivery.
The integration of technology in value-based care programs is essential for advancing the healthcare system and achieving the goals of improved patient outcomes and cost containment. As technology continues to evolve, its impact on value-based care will only grow, driving further improvements in healthcare delivery.
Point-of-Care Decision Support
Point-of-care decision support tools are crucial for delivering tailored, evidence-based recommendations directly at the site of patient interaction. These tools aid healthcare providers in making informed clinical decisions quickly by providing relevant patient-specific information in real-time. For example, OMI offers a point-of-care decision support, technology-enabled solution for all major specialties, enhancing clinical quality and improving patient outcomes.
Providing clinicians with real-time data, point-of-care decision support systems enhances clinical decision-making and ensures patients receive the right care at the right time. This technology is essential for improving the overall quality of care delivered and supporting the goals of value-based care.
Data Analytics and Patient Monitoring
Data analytics in healthcare enables healthcare providers to identify high-risk patients and tailor interventions effectively. It allows for predictive insights that improve patient management and care coordination, leading to better patient outcomes. Remote patient monitoring systems contribute to enhanced coordination and efficiency in healthcare delivery and support the principles of value-based care.
The combined use of data analytics and remote monitoring results in improved care coordination and cost-effectiveness in healthcare. Leveraging these technological advancements, healthcare providers can deliver more personalized and efficient care, further advancing the goals of value-based care programs.
Future Directions and Innovations
Value-based care strategy continues to evolve with new models being developed that promise to advance the delivery of healthcare. Technological innovations are expected to lead to further improvements in patient outcomes while also containing costs.
As the healthcare landscape continues to change, new value-based care programs and models will emerge, driving further advancements in care delivery and patient outcomes.
New VBC Programs and Models
Emerging models like direct contracting and enhanced oncology initiatives aim to improve care coordination and patient outcomes. Direct contracting arrangements are becoming a significant approach in value-based care, focusing on improving patient outcomes through better care coordination.
Enhanced oncology initiatives are designed to align financial incentives with high-quality cancer care, further advancing the goals of value-based care.
Collaboration and Integration
Collaboration among healthcare stakeholders, including providers, payers, and patients, is crucial for improving care quality and cost-effectiveness. Healthcare stakeholders such as physicians, hospitals, insurers, and community organizations must work together to develop coordinated strategies that enhance patient care and reduce costs. Integrating services across various healthcare sectors allows for a more holistic approach to patient care, minimizing gaps and redundancies.
Effective collaboration and service integration not only enhance patient outcomes but also lead to significant cost savings across the healthcare system. By working together, stakeholders can overcome the challenges of value-based care and drive further improvements in healthcare delivery.
The Promise of Personalized Medicine
Personalized medicine aims to tailor healthcare interventions based on individual patient data, enhancing the effectiveness of value-based care. Focusing on patient-centric approaches and real-time monitoring, personalized medicine can significantly improve patient outcomes and overall healthcare quality. Innovations in personalized therapies are set to reshape value-based care by providing more effective and targeted treatments for patients.
As personalized medicine continues to advance, its impact on value-based care will grow, leading to more precise and effective treatments. This approach aligns with the principles of value-based care, focusing on delivering high-quality care that meets the unique needs of each patient.
Summary
In summary, the history of value-based care is a testament to the continuous efforts to improve healthcare delivery and patient outcomes. From its early beginnings to the significant policy reforms and technological advancements, value-based care has evolved to meet the needs of patients and providers alike. Key programs and initiatives, such as the Affordable Care Act, CHIP Reauthorization Act, and Medicare Advantage Plans, have played crucial roles in shaping the landscape of value-based care.
As we look to the future, the promise of new value-based care programs and models, along with the integration of advanced technologies and personalized medicine, holds great potential for further transforming healthcare delivery. By focusing on patient outcomes and cost efficiency, value-based care continues to pave the way for a more sustainable and effective healthcare system.
Frequently Asked Questions
What was the primary goal of the establishment of Medicare and Medicaid?
The primary goal of establishing Medicare was to provide healthcare coverage for older adults, while Medicaid was created to assist individuals with limited financial resources.
How did the Affordable Care Act contribute to value-based care?
The Affordable Care Act significantly advanced value-based care by creating the Center for Medicare and Medicaid Innovation and introducing Accountable Care Organizations (ACOs), which focus on care coordination and cost control. This shift promotes improved patient outcomes and more efficient healthcare delivery.
What are the benefits of point-of-care decision support tools?
Point-of-care decision support tools significantly support clinical decision-making by delivering real-time, patient-specific information, which ultimately leads to improved patient outcomes. Their ability to assist healthcare providers in making informed decisions quickly is a crucial benefit.
How do Medicare Advantage Plans support value-based care?
Medicare Advantage Plans support value-based care by implementing models that encourage healthcare providers to prioritize quality of care over service volume, thereby improving care coordination between hospital and outpatient services. This approach ultimately aims to enhance patient outcomes and satisfaction.
What challenges do healthcare providers face in transitioning to value-based care?
Healthcare providers encounter difficulties in adapting to new payment models, aligning incentives effectively, and managing the complexities and financial risks that come with value-based care programs. These challenges can significantly impede the transition to a more effective healthcare system.